Are Pressure Injuries Burning Through Your Budget?

Everything You Need to Know About Pressure Injury Prevention & Treatment in Hospitals
- Home
- Clinical Resources
- Guide to Pressure Injury Prevention
Pressure injuries (PIs) are the bane of healthcare providers. According to the Agency for Healthcare Research and Quality (AHRQ), the rates for hospital-acquired pressure injuries increased by 6% during the period 2014–2017, despite the overall rate of hospital acquired conditions decreasing. These injuries to the skin and underlying tissue are also known as bedsores or pressure ulcers, and seem like an inevitable part of any prolonged patient stay. And when the Center for Disease Control (CDC) estimates that more than one in ten patients will develop a pressure injury, it’s reasonable to feel like there’s little you can do to turn the tide.
But we’re here to share that there is something you can do! On this page we share everything you need to know about pressure injuries and current trends in their prevention and treatment in the hospital context. This can translate to substantial savings for your healthcare facility by reducing the length of patient stays, helping you achieve your Centers for Medicare and Medicaid Services (CMS) targets, and ultimately improving patient outcomes. Learn more in our blog post, CMS Incentives Reduce HACs, But Much Work Remains.
Here’s a quick overview of what you’ll find in this guide. Use the navigation at the top of the page to jump between sections quickly.
Table of Contents
PI Types
Types of Pressure Injuries
Pressure injury definitions are tough to agree on. Ultimately, these skin and tissue injuries develop when parts of the body are subjected to extended periods of pressure against a surface.
Commonly Affected Areas and Risk Factors
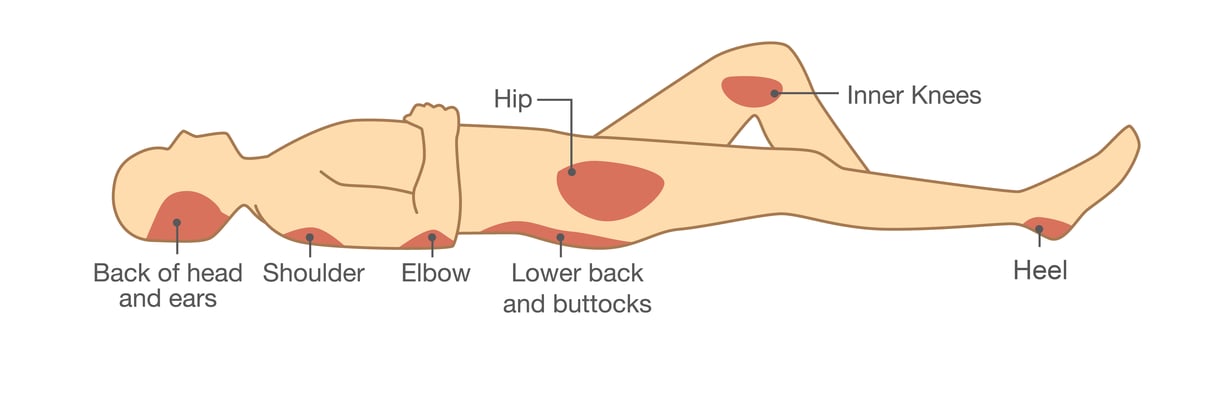
These painful lesions develop quickly on bony prominences such as the heels, hips, shoulder blades, ankles, and tailbone. If you’re treating a patient who’s temporarily immobilized due to injury, they may develop pressure injuries in these hotspots. Comorbid conditions such as reduced nerve sensation, limited mobility or poor nutritional status further increase their risk of developing a pressure injury or bedsore, and may affect its severity.
Pressure Injury Stages: How severe are they really?
Pressure injuries can be categorized into one of four stages, depending on the extent of the damage to the skin and tissue:
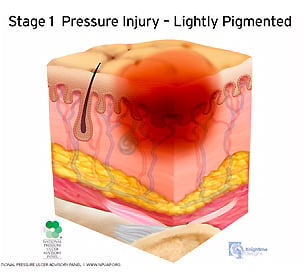
Stage 1:
Pressure injuries in stage 1 typically display non-blanchable erythema of intact skin. There can be partial-thickness loss of skin, with exposed dermis. The wound bed is pink or red, and may present as an intact or ruptured serum-filled blister.
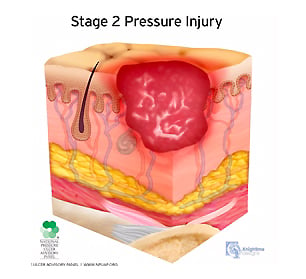
Stage 2:
Stage 2 pressure injuries present similarly to stage 1 injuries, with additional symptoms. In stage 2, granulation tissue, slough, and eschar are present.
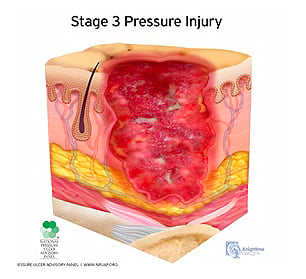
Stage 3:
A stage 3 pressure injury presents with full-thickness skin loss. Fat is visible in the ulcer, and granulation tissue and rolled wound edges are often present. Slough and/or eschar may be visible. Depth of tissue damage varies by anatomical location.
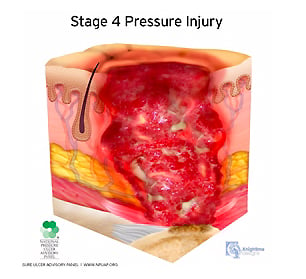
Stage 4:
A stage 4 pressure injury presents similarly to stage 3 pressure injuries, with additional symptoms. Full-thickness skin and tissue loss includes exposed or directly palpable fascia, muscle, tendon, ligament, or bone in the ulcer. Undermining and/or tunnelling often occur in addition to rolled wound edges.
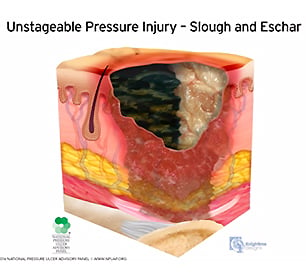
Unstageable:
An unstageable pressure injury presents as full-thickness skin and tissue loss, in which slough or eschar obscures the extent of the tissue damage within the ulcer. Once this is removed, it should reveal a stage 3–4 pressure injury.
Learn more in our blog post, A Nurse’s Visual Aid for Illustrating Pressure Injury Stages. Or if you’re wanting to share something a little less complex with a lay-person, take a look at our blog post, Simple Ways to Explain Pressure Injury Stages to Your Patients.
Cost of PIs
What Do Pressure Injuries Really Cost Healthcare Organizations?
Pressure wounds are a bigger problem than you may realize, not least because developing a pressure injury can extend the average length of a patient’s hospital stay from five days, to over eleven days. This costs the healthcare system, and your hospital, an exorbitant amount of money — according to this report by the AHRQ, hospital-acquired pressure injuries cost the industry between $9.1 and $11.6 billion during the 2014–2017 period, alone.
But pressure injuries cost more than just money, and impact more than the patient. Nurses and clinicians face pressure injuries as a clinical challenge, and your facility can face crippling PI-related litigation. According to the AHRQ, there are more than 17,000 pressure ulcer-related lawsuits filed each year.
Caring for pressure sores can be difficult and time consuming, additionally placing caregivers at risk of injuries such as back-strain and fatigue. Yet, patient care may call for the use of medical devices that increase the risk of skin injury and breakdown. This kind of balancing act is one nurses and clinicians face daily.
The holistic cost of pressure injuries, and the growing complexities in healthcare means any solution to pressure injury prevention and treatment needs to tick more than just one box. Luckily, just as hospital-acquired pressure injuries have been identified as a serious challenge, prevention and treatment methodologies have developed to address them.
Prevention and Treatment
What’s the Latest Approach to Pressure Injury Prevention and Treatment?
Great strides have been made in pressure injury treatment and prevention since early evidence of them was found on Egyptian mummies dating back more than 5000 years. While the earliest treatments focused on cleaning and bandaging the wound, we’ve now developed therapies that can support cross-functional collaboration and care. And, more importantly, developed therapies that can help prevent them occurring at all.
Interested in learning more about how pressure injury treatment has changed from ancient Egypt until today? Learn more in our blog post, The Evolution of Pressure Injury Treatment.
What Happens Today?
By implementing evidence-based standards of practice, nurses have led the charge in pressure injury prevention and care. These practices include:

Daily skin assessments, which ensure existing ulcers are accurately staged and that any new pressure injuries are quickly noted.

Proper turning and handling techniques, which protect both the patient and caregiver from injury and fatigue and help redistribute pressure.

The use of therapeutic support surfaces. Our next section shares a little more on how these can help!

Managing comorbid conditions and nutritional status. Paying close attention to these can lower the risk of developing PIs in patients with, e.g. compromised immune systems.
Patient education can engage patients actively in their own care and help achieve greater reductions in the instances and severity of pressure injuries.
With the help of the right tools and therapies that support cross-functional collaboration and care, nurses and clinicians have been able to address the medical and emotional needs of their patients. Research also shows that when patients are encouraged to become involved in their own health care, they’re more likely to adhere to treatment. This is why patient education also plays a vital role in contemporary treatment practices. Learn more in our blog post, How Nurses Can Involve Patients in Pressure Ulcer Prevention.
Nurses and clinicians are our healthcare innovators, and it’s no different when it comes to pressure injury treatment. Read more in our blog post, How Airisana® Helps Nurses Lead the Way in Pressure Injury Treatment. And find out how they’ve contributed to significant innovations in healthcare in general on our resource page, How Nurses Lead the Way in Reducing Pressure Injuries.
Alternating Air Mattresses
How Alternating Air Mattresses Can Help
Despite a readiness to play an active role in their own treatment, sometimes patients need a little extra support. And the same goes for caregivers. Alternating air mattresses are the top technology available today for exactly that. They help ease the burden of care by:
- Redistributing the pressure on the tissue loads
- Controlling microclimates
- Reducing shear forces
- Protecting against friction
- Immersion and envelopment
By using airflow to wick away moisture, leveraging an air mattress's continuous motion to rotate patients and more, caregivers can gain the support they need to treat for optimal patient outcomes. Learn more in our blog post, Five Common Uses for Therapeutic Support Surfaces. Or, dive deeper with this post that shares the key role alternating air mattresses play in the prevention and treatment of pressure injuries.
Yet most therapeutic and pressure mattresses often don’t yield the expected results. While all therapeutic support surfaces may be a step up from regular hospital mattresses, they could be leaving you with less than desirable outcomes because of design flaws such as consistent airflow, repeated pressure patterns, and the inability to support multiple treatment therapies (such as respiratory care or physical therapy).
That’s why choosing the right mattress is integral to ensuring effective pressure injury prevention and treatment. Algorithms can help clinical staff decide on the right product. They also help you prepare proposed questions to ask your supplier before making a final choice. These could include:
- Does it reduce the cost of care?
- Does it offer randomized pressure therapy modes?
- Can it offer targeted microclimate management?
- Is it easy to use by staff?
- Does it support comprehensive patient care?
- Does the design assist caregivers with turning and repositioning?
Learn more in our blog post, Support Surface Algorithms — How Confused is Your Team?
Why and How Airisana® Tackles Pressure Injury Prevention and Treatment
Because we found traditional alternating air mattresses were falling short, we went back to the drawing board and developed the Airisana® therapeutic support surface. While there’s no quick fix to the challenge of eradicating pressure injuries in our healthcare system, we made it our mission to help turn the tide by creating an alternating air mattress that checks all the boxes to those tough questions. This meant addressing drawbacks in available mattresses which included:
- Repeated pressure patterns, which increases the risk of allostasis
- Consistent airflow, which overly dries healthy skin while preventing skin breakdown in affected areas
- Care impediments as available technology wasn’t designed to suit the needs of other members of the patient care team, such as respiratory care and physical therapy.
Informed by the experiences and insights of healthcare specialists, Airisana® was designed with the transformative power of five therapies in one device. Each easy-to-use unit comes with:
- Revolutionary pressure therapy to reduce acclimatization
- Focussed airflow to match the patient’s mass distribution
- Turn-assist capabilities to reduce friction, shear risk and staff injury
- Early mobility support
- Extended battery life and an intuitive touchpad user control
- Easy-to-clean Dartex micromanagement cover that promotes infection prevention
Put the control over pressure injury prevention and treatment back into the hands of clinicians and therapists. Experience the power of Airisana® for yourself in the comfort of your own healthcare institution by clicking the button below and requesting a product evaluation. Working together we can turn the tide against pressure injuries for good, and improve patient outcomes while reducing costs to your healthcare facility.





