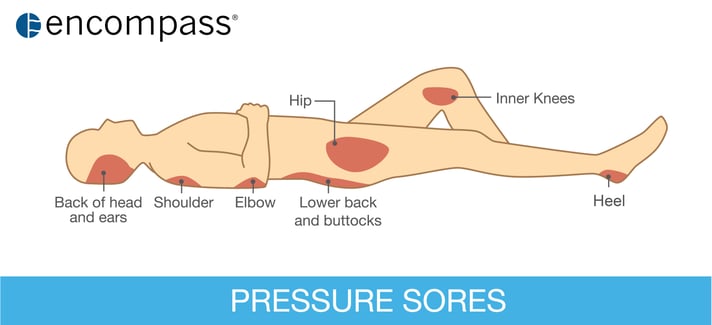
Pressure injuries (PIs), also known as bedsores or pressure ulcers, are injuries to the skin and underlying tissue that occur when parts of the body are subjected to prolonged periods of pressure against a surface such as a bed or a chair. These painful lesions can develop quickly on bony prominences including the heels, hips, shoulder blades, ankles, and tailbone in individuals who are experiencing immobility and overall poor health.
Pressure injuries are particularly problematic in long term and post-acute care (LT/PAC) facilities where the Centers for Disease Control estimates that more than 1 in 10 patients have a PI. Also, the patients who are discharged to LT/PAC facilities from acute care are more likely to have been hospitalized originally for conditions associated with a higher risk of these injuries.
Related: Pressure injury prevention & treatment strategies in healthcare facilities.
Nurses in these LT/PAC settings are routinely tasked with juggling the complex medical needs of multiple patients, many with several comorbid conditions. Their patients are very likely to have one or more of the major risk factors for PIs, which include limited mobility, reduced nerve sensation, and poor nutritional status. In addition, residents of these facilities are often older adults who suffer from chronic conditions such as diabetes, obesity, cognitive impairment, circulatory problems, and dehydration. Other Issues which can compound PI risk include incontinence and taking many daily medications, some of which can exacerbate the risk for PIs. Against this backdrop, a patient who becomes immobilized even for a few days due to a relatively minor illness such as 24-hour virus may be prone to developing a PI. Not only are these sores painful, but they also put patients at risk for further infection.
There is ample evidence that patient outcomes improve when practice standards are in place such as those in the International Pressure Ulcer Guidelines developed by the NPUAP/EPUAP. A successful program will include multidisciplinary strategies such as daily skin assessment, effective management of comorbid conditions, incontinence care, attention to the patient’s nutritional status, and safe turning and handling techniques to avoid friction injuries to the skin. A central pillar of PI prevention is the use of therapeutic surfaces to redistribute the patient’s body weight to prevent excessive pressure on areas that are most susceptible to PIs. The most effective of these provide the highest total skin contact coupled with the lowest degree of pressure on particularly vulnerable points such as the tailbone, hips, ankles, and heels.
Given that a large portion of patients in LT/PAC are at high risk for pressure injuries due to their level of immobility and coexisting conditions, special care needs to be taken in choosing the right therapeutic surface for this setting. The Airisana™ Therapeutic Support Surface incorporates innovations such as randomized pressure therapy treatment algorithms, which help significantly reduce acclimation, and unique valve technology for targeting airflow to the places where the highest pressure, heat and moisture build is indicated. The design of the Airisana™ surface is also compatible with the delivery of other types of bedside care often needed for these patients. To learn more about the Airisana™ surface click here.


