
Hospital-acquired pressure injuries (HAPIs) pose a serious health risk to patients in both acute and long-term care settings. More than one million patients in these facilities develop pressure injury (PI) each year. Advanced pressure injuries can be extremely painful and debilitating. The development of a PI will increase the average length of the patient’s hospital stay from 5 days to over 11 days. PIs are also directly responsible for roughly 60,000 patient deaths each year. Additionally, the cost of PIs takes a heavy financial toll on the U.S. healthcare system. In this report by the AHRQ puts total yearly price tag for these mostly avoidable injuries to be between $9.1 and $11.6 billion.
A pressure injury can be described as localized damage to the skin and underlying soft tissues, most often over a bony prominence or the site of a medical device.
Related: See our resource on pressure injury prevention & treatment in healthcare facilities.
Starting with the initial skin assessment of a patient’s skin upon entering the hospital, and continuing throughout their stay, it is critically important for the clinical staff to properly identify the earliest signs of PIs. To further this goal, the National Pressure Ulcer Advisory Panel (NPUAP) issued a report in 2016 called, NPUAP Pressure Injury Stages, in which they redefined the stages of pressure injuries.
Within this definition, PIs can be further categorized by the extent of damage to the skin and tissue.
-
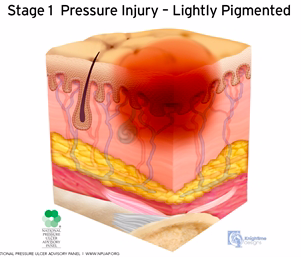
Stage 1:
-
Non-blanchable erythema of intact skin. Partial-thickness loss of skin with exposed dermis. The wound bed is viable, pink or red, moist, and may also present as an intact or ruptured serum-filled blister. Fat and deeper tissues are not visible. Granulation tissue, slough, and eschar are not present.
-
-
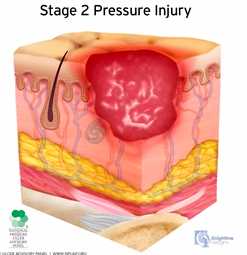
Stage 2:
-
Partial-thickness skin loss with exposed dermis. Partial-thickness loss of skin with exposed dermis. The wound bed is viable, pink or red, moist, and may also present as an intact or ruptured serum-filled blister. Fat and deeper tissue is not visible.
-
-
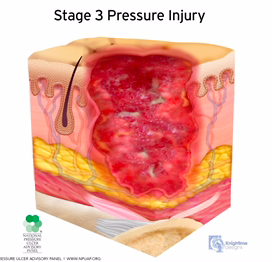
Stage 3:
-
Full-thickness skin loss. Full-thickness loss of skin, in which fat is visible in the ulcer, and granulation tissue and rolled wound edges are often present. Slough and/or eschar may be visible. The depth of tissue damage varies by anatomical location.
-
-
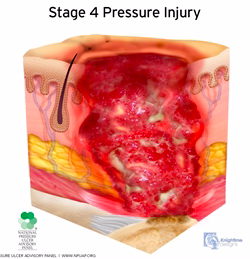
Stage 4:
-
Full-thickness skin and tissue loss. Full-thickness skin and tissue loss with exposed or directly palpable fascia, muscle, tendon, ligament, cartilage or bone in the ulcer. Slough and/or eschar may be visible. Rolled wound edges, undermining and/or tunneling often occur.
-
-
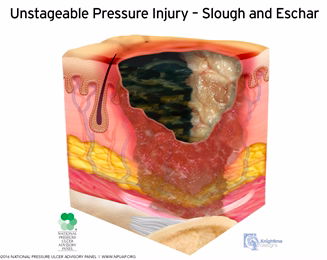
Unstageable:
-
Obscured full-thickness skin and tissue loss. Full-thickness skin and tissue loss in which slough or eschar obscures the extent of tissue damage within the ulcer. Removal of slough or eschar will reveal a Stage 3 or Stage 4 pressure injury.
-
-
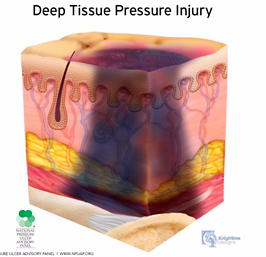
Deep Tissue:
-
Persistent non-blanchable deep red, maroon or purple discoloration. Intact or non-intact skin with localized area of persistent non-blanchable discoloration or epidermal separation revealing a dark wound bed or blood-filled blister.
-
-
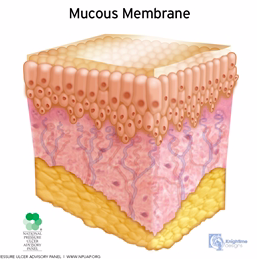
Mucosal Membrane:
-
A pressure injury is that occurs on mucous membranes in a location where a medical device has been used. Due to the anatomy of the tissue, these ulcers cannot be staged.
-
Medical Device Related:
-
Pressure injury resulting from the use of diagnostic or therapeutic devices. The injury most often reflects the shape of the device. These injuries should be staged using the staging system.
-
-
To prevent the occurrence of new PIs and promote the healing of existing wounds, a therapeutic support surface must reduce excess pressure on vulnerable areas of the body and control the skin’s microclimate to eliminate excess moisture and humidity. To address these challenges, the Airisana™ therapeutic support surface incorporates sophisticated technologies such as randomized pressure therapy algorithms, and a unique valve system that targets airflow to where it is most needed. In addition, Airisana™ was designed to safely facilitate bedside therapy without hindering the multiple disciplinary care a patient often needs. Click here to learn more about how Airisana™ can aid in the prevention of HAPIs.


